by Joan Haynes, NMD
Still think 1200 mg of calcium daily will build good bone? Think again. That much calcium might only not help, but actually harm. Excessive calcium might compromise cardiac and kidney health. Here’s a fresh look at osteoporosis and the host of minerals, cofactors, diet and lifestyle recommendations that are necessary for good bone health.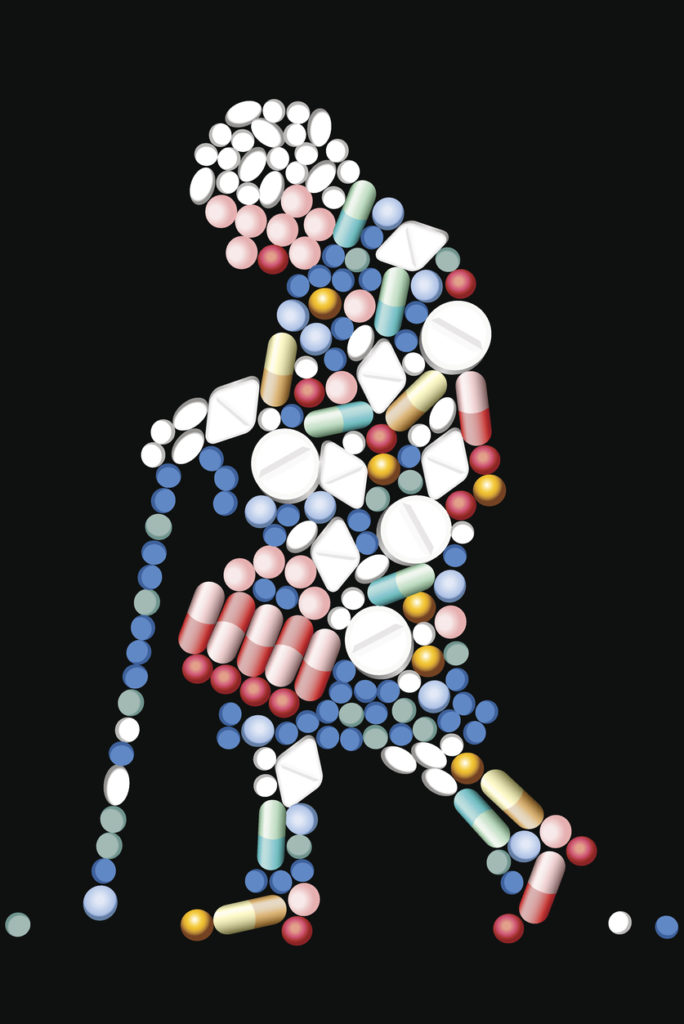
Careful with Calcium
Health professionals are beginning to question the recommendations on calcium supplementation. A study published in the British Medical Journal in 2008 showed a positive correlation between calcium supplementation and an increased risk of myocardial infarction (heart attack) in older women through calcification of coronary arteries. Other studies showed too much calcium leads to deposits in the kidneys leading to kidney stones.
Not All Calcium is the Same
The type of calcium is always important to consider. At BNH we recommend calcium citrate or calcium citrate-malate. These are highly absorbable forms of calcium and we recommend that women stay under 500 mg a day. The popular and inexpensive calcium carbonate form is what chalk and Tums are made from. Calcium carbonate actually blocks its own absorption through buffering stomach acid.
Low Stomach Acid
You might be getting plenty of calcium and other minerals in your diet, but if you don’t have enough stomach acid to break them down, you can’t absorb them. Symptoms of low stomach acid might be acid reflux, heartburn, burping, gas, bloating, and nausea. Low stomach acid is associated with an inability to digest meat well and often people’s stomach feels heavy or overly full after meals, despite eating a normal amount. Sometimes, even if there are no gastrointestinal symptoms, it is useful to screen patients for low HCL if they have poor mineralization health conditions, such as those with anemia, osteoporosis, thinning hair, thin nails, and nervous system problems like insomnia, anxiety, and restless leg syndrome. READ MORE about low stomach acid in an article on our web page.
Bones are MUCH More than Calcium
To build and maintain bone we must also have optimal amounts of vitamin D, vitamin K, magnesium, potassium and essential trace minerals such as boron. Adequate protein is also needed as well as omega-3 oils.
High Calcium Foods are High Mineral Foods
We all know that dairy foods are high in calcium, but many of our patients avoid dairy. The best food sources of calcium, other than dairy, include whole grains, beans, almonds and other nuts, dark green leafy vegetables like kale, bok choy and turnip greens, also salmon and sardines. It is interesting to note that individuals who avoid dairy due to lactose intolerance do not experience a corresponding increase in osteoporosis.
A Word about Strontium
In my patients that have demonstrated bone loss with a DEXA scan, I recommend the mineral strontium citrate. This mineral has been shown to increase bone density. Caution: calcium will inhibit the absorption of strontium if taken together so they must be ingested at different meals.
Alkaline Diet
A diet high in animal protein, grains, and sugar and low in vegetables and fruit can cause an increase in urinary excretion of calcium, leading to bone loss. These foods acidify your system, causing a leaching of calcium from the bone to keep your body’s pH normal. A whole-foods, plant-based diet create a more alkaline environment.
Exercise
Always at the top of the list to build and maintain healthy bones is exercise. Both weight bearing and cardio together have been shown to be the most effective.
Don’t Wait to Take Bone Health Seriously
About one in two women over the age of 50 will develop osteoporosis but what is often overlooked is one in four men over the age of 50 will also develop the disease. Be proactive with your bone health.
At Boise Natural Health, we can help you design an effective bone health program that includes individualized supplementation and overall health optimization. Call today to make an appointment 208-338-0405.
