Many people are aware that sex hormones like estrogen, progesterone, testosterone, and DHEA influence more than just reproduction and menstrual cycles. While common knowledge acknowledges their impact on bone density, brain health, and cardiovascular risk, emerging medical perspectives recognize that these hormones have even broader effects.
Our Changing Brain Architecture Throughout the Menstrual Cycle
Recent studies have revealed intriguing insights into how the architecture of our brains changes during different phases of the menstrual cycle. These hormonal brain differences could potentially explain the increased incidence of early-onset dementia in women who experience early menopause. These new studies suggest that our thought processes may also vary depending on the cycle phase, potentially influencing behavior. Hormonal fluctuations and physical changes in the brain may contribute to reported instances of “brain fog” at specific points in the menstrual cycle. Although some studies indicate no difference in task performance, patients often report changes in effort. Animal models also suggest increased brain connections before ovulation, aligning with women’s experiences of feeling their best during this period. This research opens new avenues for exploring the validation of reported brain changes throughout the menstrual cycle.
The Impact of Menstrual Cycles on Immunity
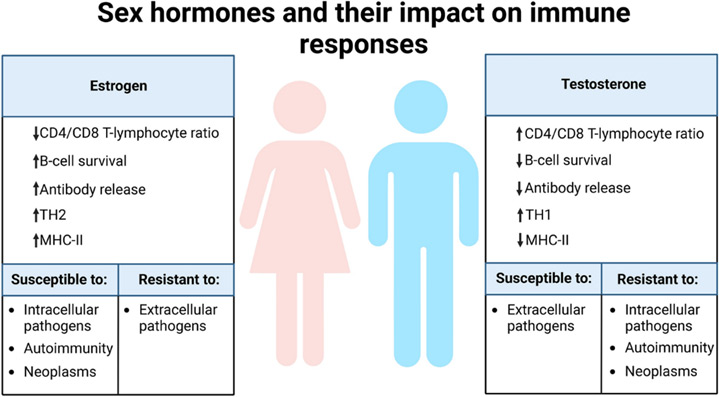
Surprisingly, a Long COVID study delved into the sex differences and hormonal influences on the immune system. Hormonal fluctuations during menstruation, early follicular phase, and PMS (end luteal phase) favor the TH1 immune pathway, which is effective against viruses but can escalate inflammation, autoimmunity, and cancer risk. This phase also leaves individuals susceptible to bacterial and parasitic infections. Conversely, during the late follicular phase, ovulation, and luteal phase (higher estrogen and progesterone levels), women favor the TH2 immune pathway. While this pathway protects against parasites and bacteria and is anti-inflammatory, it may enable stealth viruses to replicate. These immune system changes potentially explain the higher incidence of autoimmune diseases in women, with patients often reporting flares of symptoms around ovulation.
In summary, we are entering an exciting era of research that focuses on the monthly changes experienced by females, recognizing that these changes extend beyond reproduction to impact the entire body. The evolving understanding of these hormonal dynamics is poised to reshape the field of medicine.
References:
- https://www.washingtonpost.com/wellness/2023/11/30/women-brain-menstrual-cycle-changes/
- https://www.nature.com/articles/s44220-023-00125-w
- https://www.biorxiv.org/content/10.1101/2023.10.09.561616v1?et_rid=294001483&et_cid=4942736
- https://www.nature.com/articles/s41386-019-0435-3
- https://link.springer.com/article/10.1186/s12967-023-04515-7